Curious about cutting-edge treatments for challenging mental health conditions? Enter Ketamine Assisted Psychotherapy KAP — a dynamic approach blending ketamine’s neuromodulatory effects with the transformative power of psychotherapy. Without claiming a cure-all, this article offers a critical assessment of KAP’s potential, backed by scientific insights and patient experiences, guiding those in need towards an informed decision.
Understanding Ketamine Assisted Psychotherapy (KAP)
Ketamine Assisted Psychotherapy (KAP) is a novel therapeutic approach that combines ketamine, a potent anesthetic, with psychotherapy to manage mental health conditions like depression, anxiety, and PTSD. This potent combination has shown promise in providing rapid alleviation of symptoms associated with these mental health disorders, leading to swift enhancements in mood and emotional resilience.
KAP psychotherapy sessions aim to encourage long-lasting benefits and significant life changes, taking advantage of the mood and cognitive improvements induced by ketamine during a psychotherapy session.
The Role of Ketamine in KAP
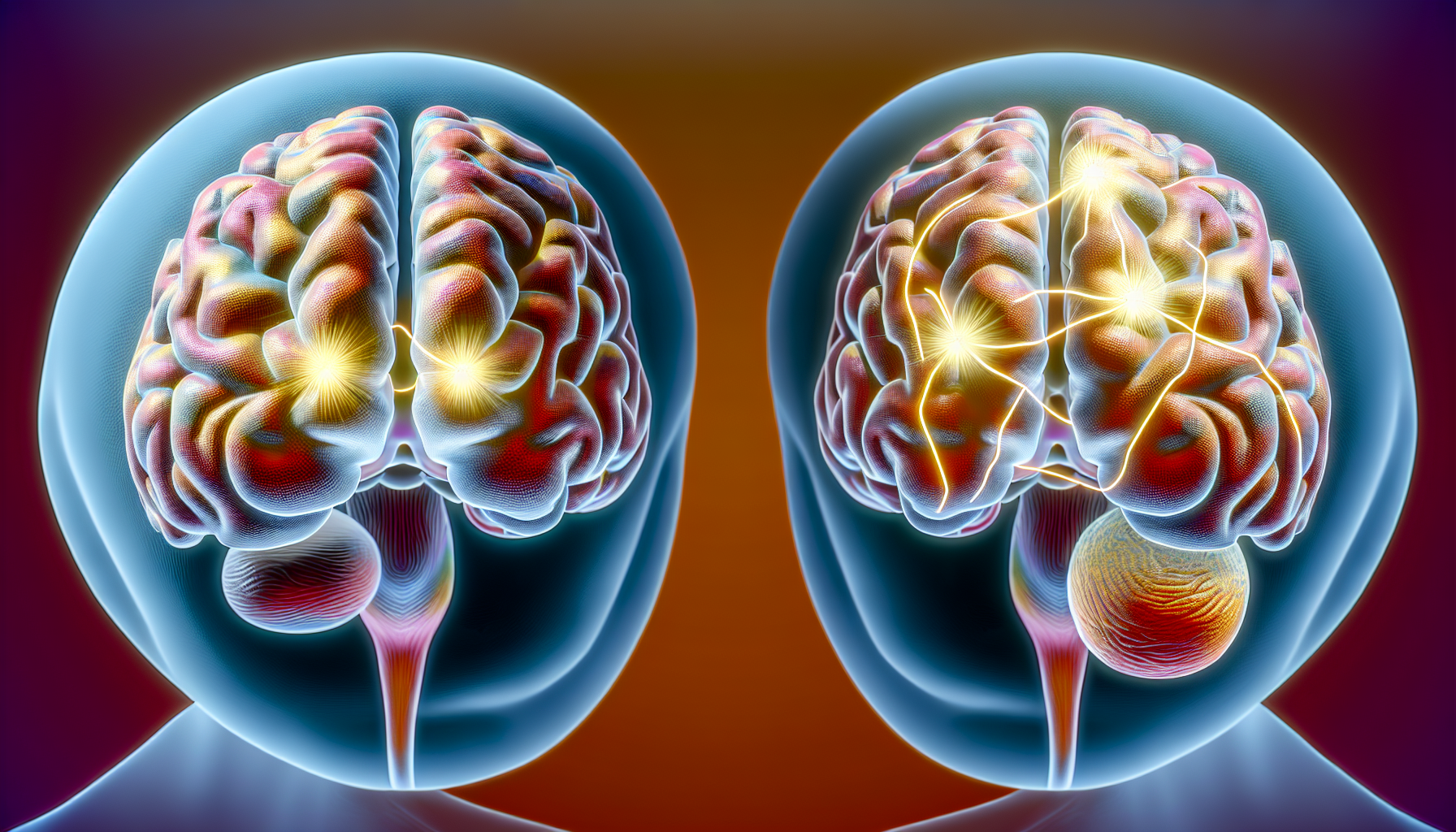
Ketamine plays a significant role in KAP by inhibiting a fraction of NMDA receptors, a mechanism that has been found to regulate anxiety-like behaviors. This potent anesthetic facilitates neuroplasticity by promoting the regeneration of synapses and restructuring the brain — critical components of recovery in mental health interventions.
Ketamine rapidly alleviates depression symptoms and, in conjunction with psychotherapy, amplifies the overall effectiveness of KAP.
Synergy Between Ketamine and Psychotherapy
KAP unites ketamine and psychotherapy, a union often known as a drug-sparing treatment paradigm, providing a combined approach to address mental health disorders. The effectiveness of KAP can be enhanced by increasing the doses of ketamine, conducting more frequent KAP sessions, and extending the duration of psychotherapy.
Cognitive Behavioral Therapy (CBT) and Mindfulness-Based Interventions (MBI) are commonly utilized in KAP as sequenced treatment alternatives, with the median number of psychotherapy sessions being 11.
Suitability for Treatment-Resistant Depression
KAP is particularly well-suited for patients with treatment-resistant depression and chronic mental health conditions, providing an alternative to conventional therapies. KAP merges ketamine and psychotherapy to cater to the needs of patients who have found traditional treatments ineffective, including those suffering from major depressive disorder.
The efficacy of KAP in treating treatment-resistant depression varies, with studies indicating improvement rates ranging from 41% to 86%.
The Science Behind KAP’s Effectiveness
KAP’s effectiveness can be attributed to several factors. The rapid antidepressant effects of ketamine play a crucial role, offering immediate relief to patients with clinical depression. Ketamine is also found to enhance neuroplasticity through signaling pathways such as mammalian targets of rapamycin (mTOR), glycogen synthase kinase-3 (GSK3), and elongation factor 2 (eEF2) kinase.
As an NMDA receptor antagonist, ketamine boosts synaptic excitability and synaptogenesis, laying the foundation for the noticeable neuroplasticity benefits.
Ketamine’s Rapid Onset Antidepressant Effects
A key feature of KAP is ketamine’s quick-acting antidepressant effects, bringing instant relief from depressive symptoms. This is a significant contrast with the delayed onset of traditional treatments.
Ketamine’s effects become apparent immediately after administration and can last for up to a month, a stark contrast to traditional treatments, which typically have a more delayed onset.
Long-Term Benefits and Neuroplasticity
In addition to its immediate impact, KAP encourages lasting benefits by enhancing neuroplasticity and augmenting levels of brain-derived neurotrophic factor (BDNF). The presence of BDNF in the brain mitigates the impacts of acute and chronic stress and is essential for the enduring advantages of KAP. By interacting with the TrkB receptor and stimulating synaptic spine density via the Ras/ERK pathway, BDNF promotes neuroplasticity.
Elevated BDNF levels have been linked to enhanced cognitive function and reduced severity of psychiatric conditions, highlighting the enduring advantages of BDNF on mental health, including mental health issues.
Addressing Chronic Neuropathic Pain and PTSD
In addition to its efficacy in treating depression, KAP has demonstrated potential in addressing chronic neuropathic pain and PTSD. In a study involving patients with chronic pain, a 5-day IV ketamine course led to notable pain reductions in over half of the patients.
Further, KAP has been found to effectively disrupt the reconsolidation of dysfunctional memories associated with trauma, leading to a reduction in the symptom burden of PTSD. The ability of ketamine to reduce inflammation in the brain and disrupt the pathological reconsolidation of traumatic memories are mechanisms that help alleviate chronic neuropathic pain and PTSD symptoms.
The Journey of a Ketamine Therapy Session
A typical ketamine session consists of preparation, administration of ketamine, and aftercare, all aimed at guiding patients through a transformative journey of self-exploration and healing. Ketamine is administered via an injection in the arm muscle or sublingually, and the patient is provided with an eye mask and listens to music while receiving support from a therapist during the administration.
A session can last for a maximum of three hours.
Preparing for Your Session
Prior to commencing treatment, individuals are required to assess if ketamine therapy is suitable for their needs, taking into account their medical and psychiatric conditions. The therapist’s role in preparing a patient for a KAP session encompasses:
- An initial consultation
- Preparation sessions
- KAP dosing sessions
- Integration sessions
- Follow-up sessions
The establishment of a supportive environment is crucial in ensuring the comfort and safety of the patient throughout the experience.
During the Ketamine Administration
During the ketamine administration, the therapist’s responsibility is to provide guidance to the patient, assisting them in managing difficult emotions and altered perceptions. Ketamine has the potential to induce altered sensory perceptions, resulting in heightened vividness of colors and increased sensitivity to noises, which at lower doses may elicit pleasure and facilitate a more impartial outlook on the patients’ lives.
The dissociative effects of ketamine are indicative of its therapeutic influence on network connections linked to rumination and are managed through a dosage escalation approach facilitated by KAP.
Aftercare and Integration
Aftercare and integration hold significant importance in KAP. Aftercare offers a support system for individuals who may encounter emotional experiences during the therapy, while integration assists individuals in comprehending and applying the insights gained during the therapy to their daily lives. Aftercare practices such as self-care, maintaining hydration, and engaging in reflective activities like journaling or meditation aid in emotional processing and the integration of therapy insights.
Integration is pivotal in understanding experiences from KAP, helping individuals interpret and apply the insights gleaned from the ketamine experience to their daily lives.
Risks and Considerations in KAP
Despite the potential benefits of KAP, it’s vital to understand the associated risks and considerations. Patient safety during KAP can be ensured by:
- Implementing comprehensive safety policies and procedures
- Facilitating transformative experiences
- Offering support and guidance during distress
- Fostering a secure and trustworthy therapeutic environment.
Potential side effects such as altered mental status, hallucinations, dizziness, and nausea should be discussed with patients prior to treatment.
Managing Dissociative Effects
The dissociative effects of Ketamine in KAP encompass feelings of detachment, derealization, and depersonalization. Therapists assist in managing these effects through the use of psychotherapy, which serves to extend the positive effects of ketamine and establish a therapeutic setting.
Methods utilized in KAP to navigate altered states of consciousness encompass the psychometric assessment of these states and honoring the autonomy of patients in their altered experiences.
Understanding the Side Effects
Potential side effects of KAP include nausea, vomiting, and agitation. However, these side effects manifest only in a minority of patients and are typically transient.
There are also more severe side effects like:
- disorientation
- confusion
- loss of motor coordination
- dizziness
- increased blood pressure
- increased heart rate
- changes in breathing
- painful or difficult urination
- increased urination
- loss of bladder control
- blood in urine
- light-headedness
Ensuring Patient Safety
Promoting patient safety in KAP entails:
- A thorough evaluation of the patient’s mental health background and present symptoms
- The execution of specific protocols to enable transformative experiences, provide comfort during distress, and stimulate positive therapeutic results
- Patients completing a self-administered questionnaire on KAP during the pre-, immediate, and post-intervention stages to ensure patient safety.
Healthcare professionals closely monitor patients during ketamine therapy sessions to ensure their safety, including routine checks of vital signs, mental status, and prompt addressing of any adverse effects.
Personalizing KAP: Tailoring Treatment to the Individual
KAP is not a one-size-fits-all treatment. It involves:
- Assessing patient eligibility
- Customizing dosage and frequency
- Continually monitoring and adjusting treatment plans to optimize outcomes based on individual needs.
Assessing Patient Eligibility
Patient eligibility for KAP is determined based on specific inclusion criteria such as age and diagnosis of Treatment-Resistant Depression, and exclusion criteria like active substance abuse. A comprehensive assessment of the patient’s medical history, including past illnesses, surgeries, and genetic disorders, is also critical to personalize the treatment and ensure any potential risks are identified.
The patient’s prior mental health history significantly influences their eligibility for KAP. The patient’s current psychiatric status is also a significant factor in determining their suitability for KAP.
Customizing the Dosage and Frequency
The dosage of Ketamine in KAP is determined based on its psychoactive properties at higher doses, which are believed to aid psychotherapy. The frequency of ketamine administration in KAP may vary, encompassing:
- Multiple treatments per week
- More frequent sessions during acute symptoms
- Periodic maintenance treatments, customized to the specific needs of each individual.
Modifications in ketamine dosage and frequency in KAP are determined by efficacy during a ketamine dosing session, with greater doses and more frequent sessions, as well as extended psychotherapy durations, demonstrating heightened effectiveness.
Continual Monitoring and Adjustment
Constant monitoring is a significant aspect of KAP, aiding in preventing any negative events from being missed and enhancing the safety and effectiveness of the treatment. Patients undergoing KAP therapy are generally monitored by at least two therapists during in-office sessions and subsequent monitoring, with each session lasting up to three hours.
Physicians modify ketamine doses in KAP treatment by:
- considering the individual’s reactivity to ketamine
- evaluating the efficacy of the initial dose
- tailoring the therapy to the patient’s specific requirements.
Real-world Outcomes: Success Stories and Clinical Data
Real-world outcomes of KAP include clinical data showcasing its effectiveness as an effective treatment for conditions like heroin and cocaine addiction. Additionally, there are success stories and testimonials from patients who have derived substantial benefits from the treatment.
Clinical studies, such as the one carried out by Krupitsky et al, have indicated that elevated doses of ketamine in conjunction with psychotherapy can lead to notable rates of heroin abstinence.
From Clinical Trials to Clinical Practice
Growing evidence from clinical trials has enabled the integration of ketamine treatment into clinical practice, as seen in the inclusion of multiple ketamine sessions in clinical environments. Although both clinical trials and real-world practices utilize KAP for addressing pain, mental health, and substance abuse disorders, clinical trials are primarily oriented towards showcasing the therapeutic advantages of integrating psychotherapy with ketamine treatment, while real-world practice offers perspectives on the pragmatic potential of KAP.
Patient Testimonials and Case Studies
Testimonials from patients underscore the positive impact of KAP on mental well-being, with improvements noted in mood and cognitive performance for individuals coping with conditions such as depression, anxiety, PTSD, and addiction. Several successful implementations of KAP have been documented, including higher doses of ketamine facilitating psychotherapy sessions, the use of ketamine as an adjunct in the treatment of treatment-resistant PTSD, and a treatment regimen that integrated ketamine infusions with KAP and psychotherapy to reduce suicidality and treatment-resistant depression.
Analyzing Relapse Rates and Longevity of Results
The relapse rates following KAP vary, with some patients relapsing anywhere from 18 days to 12 weeks after the final ketamine infusion. The effectiveness of KAP results typically lasts for at least 2 weeks, with sustained efficacy for up to 6 months. When higher doses of ketamine are administered, the frequency of KAP sessions is increased, and psychotherapy is extended, which can extend the effectiveness in comparison to other treatments.
Several studies indicate the long-term effectiveness of KAP, demonstrating its benefits in the treatment of conditions such as affective disorders, including:
- Depression
- Anxiety
- Post traumatic stress disorder
- Chronic pain/MDD comorbidity
Approximately 60% of patients maintain their response at 8 weeks.
Summary
Ketamine Assisted Psychotherapy (KAP), offered by leading psychologists and psychotherapists in San Francisco, California, is a groundbreaking approach for treating various mental health conditions. Currently the Bay Area CBT Center offers ketamine assisted psychotherapy in San Francisco to current clients only. KAP provides rapid symptom relief and fosters long-term neuroplasticity. Alongside KAP, the Center offers individual psychotherapy in the Bay Area, group counseling in the Bay Area, online counseling in California, and couples counseling, workshops, retreats, and online courses.
The treatment journey at the Center, encompassing preparation to aftercare, is crafted to facilitate a transformative journey of self-exploration and healing. With its potential benefits and impressive real-world outcomes, KAP, combined with the comprehensive services of psychotherapy in San Francisco, shines as a beacon of hope for those battling mental health challenges.